Submitted by: Sara M. Foster, RN, MPH, Greystone
Article taken from 2020 CEC
Remote patient monitoring (RPM) has been around for at least a couple of decades. However, the advent of smart devices—smartphones, smartwatches, etc.—brought about new capabilities and technology that have increased the quality and availability of remote monitoring. The COVID-19 pandemic made RPM even more important when lockdowns limited access to non-urgent healthcare.
What is RPM?
It is the use of some sort of electronic device, such as a smartwatch or fitness tracker, to collect physiological data from a patient—heart rate/rhythm, blood pressure, weight, etc.—and send the data to the patient’s healthcare provider. The provider can review the data to spot any changes in the patient’s status and if there are concerns, can notify the patient to address the concerns. This process can improve health outcomes.
How Does RPM Work?
The provider determines a patient’s monitoring needs and which device is appropriate for those needs. The patient is given the device by the provider or is given a prescription to obtain the device elsewhere. Once the device is connected, the patient's data is transmitted to the provider. The patient’s data is monitored and verified with the patient. Any abnormal data is sent to the provider for further review and possible intervention.
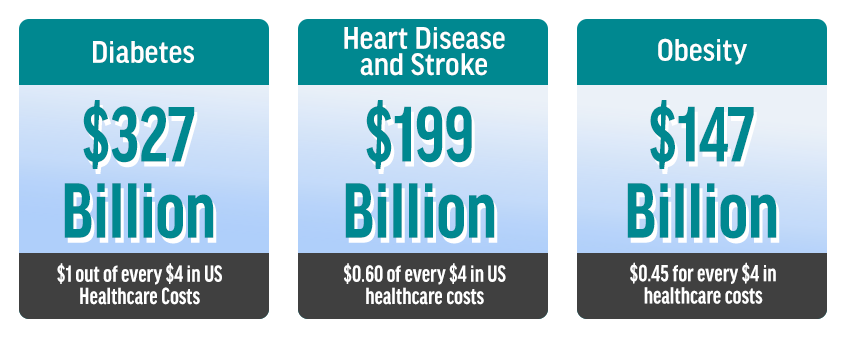
Why is RPM Important? According to Charu G. Raheja, Ph.D., CEO, TriageLogic, RPM is a key component in treating patients with chronic diseases. In the US, chronic diseases are the leading causes of death and disability and are leading drivers of the $3.5 trillion in annual overall healthcare costs. Six in 10 US adults have a chronic disease and four in 10 have two or more chronic diseases. The most common chronic diseases are diabetes, obesity and heart disease, but mental health conditions are in line to become the fourth most common chronic condition.
As an illustration of the importance of RPM, Raheja cited the example of her father. With a history of asthma, diabetes and high blood pressure, he would have been a good candidate for RPM. He began to complain of some vague GI symptoms but passed them off as being related to a recent change in diet due to visiting family, eating out a lot and eating differently than usual. After a period of travel, he returned to his hotel, where he suffered a massive heart attack and died. Had he been monitored, it’s possible a change in his condition could have been detected and he could have been referred to care by a clinician, thus possibly preventing his catastrophic event.
 Chronic Care Costs:
Chronic Care Costs:
 Benefits of RPM:
Benefits of RPM:
- Patient safety and convenience—provider receives vitals and other data regularly with fewer in-person visits
- Compliance—patients are encouraged to measure their status regularly and submit their data to their provider
- Improved health outcomes—by tracking health information and seeing trends, providers can intervene earlier, which leads to better outcomes.
Chronic Disease Example of RPM:
Congestive heart failure (CHF)—management of this disease requires frequent monitoring of various physiological parameters, such as:
- Echocardiogram—to monitor and assess heart function, the size and shape of the heart, how well the valves and heart chambers are working and more
- ECG or EKG—to monitor and assess the heart's rhythm and electrical activity
- Oxygen saturation (pulse oximetry or pulse ox)—measures the amount of oxygen in the blood
- X-ray—evaluates the lungs, which can be directly affected by the heart's functional status
- Weight—in CHF, patients are instructed to weight themselves daily and report any weight gain or loss above a certain amount.
The Call Center’s Role
There are several functions that can be provided by call center staff and triage nurses before the physician becomes involved. Non-clinical staff can:
- Review alerts regularly. Not all alerts require clinical intervention, but they do need to be tracked so that alerts that do require clinical attention/intervention can be passed on to the physician.
- Call patient back in case of device malfunction or to provide education related to proper use or positioning of the device.
- Refer alerts to a physician based on pre-determined rules.
- Assess general symptoms using symptom-based protocols
- Use device—and disease—specific protocols developed by clinicians according to the practice standards of their physician practice, hospital/health system, etc.
- Use nurse triage software to document and record calls, as well as to send a summary of the encounter to the EMR and to the provider, if needed.
- By using protocols to manage patients, triage nurses can decrease up to 50 percent of follow-up visits to physicians.
What Are Some Challenges That Organizations Face With RPM?
Finding a device that will work well for the patient, is easy to use and provides the necessary data.
It can be difficult to monitor the data, e.g., when there are too many alerts to monitor.
Costs—CMS has recently added new codes to allow providers to be reimbursed for RPM. Other payers are looking at this as well.